Does insurance cover nose job with deviated septum? This question is crucial for many considering surgery to correct a deviated septum. Insurance coverage for cosmetic procedures is often complex, and a deviated septum, while often a medical issue, can also have cosmetic implications. Understanding the nuances of medical necessity versus elective procedures, and how insurance companies define those terms, is essential to navigating this process.
This comprehensive guide explores the factors that influence insurance decisions, examines the medical necessity of a deviated septum correction, and details the process of submitting an insurance claim. We’ll also differentiate between medical and cosmetic rhinoplasty, providing clarity on when a nose job might be covered.
Understanding Insurance Coverage
Insurance coverage for cosmetic procedures, like nose jobs, varies significantly depending on the specific policy and the procedure’s classification. Understanding the nuances of health insurance plans and the factors influencing coverage decisions is crucial for patients considering such procedures. This section will delve into the intricacies of insurance coverage for nasal procedures, distinguishing between medically necessary and elective interventions.
Types of Health Insurance Plans and Coverage Policies, Does insurance cover nose job with deviated septum
Different health insurance plans have varying coverage philosophies. Some plans may cover medically necessary procedures related to a deviated septum, while others may not cover cosmetic procedures at all. PPO (Preferred Provider Organization) plans often offer more flexibility in choosing providers but may have specific guidelines for cosmetic procedures. HMO (Health Maintenance Organization) plans may have a network of doctors and procedures that are covered, but the extent of coverage can vary.
Medicare and Medicaid plans often have specific criteria for coverage, primarily focusing on procedures with clear medical necessity.
Factors Influencing Insurance Decisions
Insurance companies carefully evaluate the necessity of a procedure. Factors like the patient’s medical history, the severity of the deviated septum, and the proposed treatment plan all play a significant role in the insurance company’s decision-making process. The physician’s documentation, justifying the procedure’s medical necessity, is also critical. Insurance companies may require specific pre-authorization forms and diagnostic imaging to support the need for the procedure.
Medically Necessary vs. Elective Procedures
Procedures deemed medically necessary are those required to address a diagnosed medical condition, like a severely deviated septum causing breathing problems or chronic sinusitis. These procedures are often covered, at least partially, by insurance. In contrast, elective procedures, such as cosmetic rhinoplasty, are performed to enhance appearance and are typically not covered by insurance. The line between medically necessary and elective can be blurry in cases of nasal reconstruction, and the physician’s justification is critical in such instances.
Coverage for Nasal Reconstruction vs. Cosmetic Rhinoplasty
Nasal reconstruction procedures, often necessitated by trauma or birth defects, are more likely to be covered by insurance. The procedure’s purpose is to restore function and address a medical issue. Cosmetic rhinoplasty, aiming to improve aesthetic appearance, is less likely to receive full coverage. The extent of coverage may depend on the severity of the breathing problems associated with the deviated septum.
Insurance companies may offer partial coverage for medically necessary components of a procedure, like correcting the deviated septum, but not the cosmetic aspects.
Insurance Company Definitions of “Medically Necessary”
Insurance companies often have specific criteria for determining medical necessity. These criteria might include the presence of documented breathing difficulties, chronic pain, or other health concerns directly linked to the deviated septum. A physician’s detailed report emphasizing the functional limitations caused by the deviated septum is crucial for justifying the necessity of the procedure.
Physician’s Documentation and Justification
A physician’s comprehensive documentation is essential to justify the medical necessity of a deviated septum correction. The documentation should thoroughly describe the patient’s symptoms, medical history, and the functional impairment caused by the deviated septum. The physician should clearly explain why the procedure is medically necessary to address the specific patient’s needs, and not simply for cosmetic enhancement.
Diagnostic imaging, like X-rays or CT scans, demonstrating the severity of the septal deviation, should be included in the documentation. This detailed documentation is critical in persuading insurance companies of the procedure’s necessity.
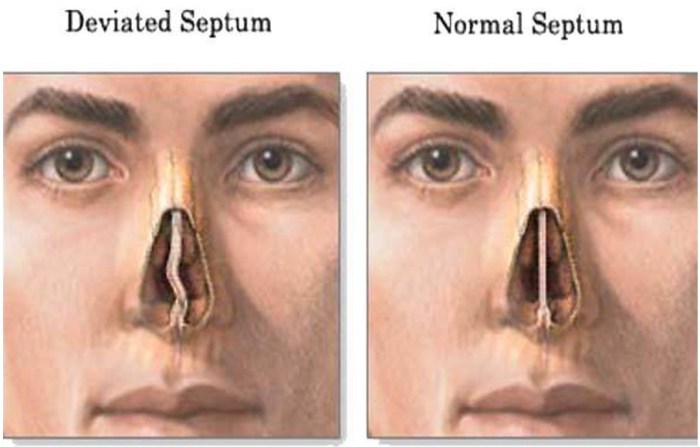
Deviated Septum
A deviated septum is a common nasal condition where the cartilage and bone that form the nasal septum are not straight. This structural asymmetry can significantly impact nasal airflow and, in some cases, necessitate medical intervention. Understanding the medical necessity behind a deviated septum correction is crucial for patients and healthcare providers alike.
Medical Conditions Necessitating Correction
A deviated septum can lead to various medical conditions that affect breathing and overall well-being. Chronic nasal congestion, sleep apnea, and recurrent sinusitis are just some of the possible consequences. These conditions often require a thorough evaluation by a healthcare professional to determine the extent of the deviation and its impact on the patient’s health.
Symptoms and Diagnoses Leading to Medical Necessity
Several symptoms and diagnoses can indicate the need for a deviated septum correction. These include chronic nasal obstruction, difficulty breathing through one or both nostrils, snoring, and frequent nosebleeds. Further, a diagnosis of sleep apnea, sinusitis, or recurrent upper respiratory infections may necessitate a deviated septum correction. Radiographic imaging, such as nasal endoscopy and CT scans, is often employed to accurately assess the degree of deviation and its potential impact on breathing.
Diagnosis and Impact on Breathing
Diagnosing a deviated septum involves a comprehensive evaluation of the patient’s symptoms and medical history. Physical examination of the nasal passages is crucial. Nasal endoscopy allows visualization of the nasal cavity and septum. CT scans provide detailed images of the nasal structure, aiding in the assessment of the severity of the deviation. The impact on breathing can vary depending on the degree of deviation.
In mild cases, breathing difficulties might be subtle, while severe deviations can lead to significant airflow obstruction, impacting the patient’s quality of life.
Impact on Breathing and Quality of Life
A deviated septum can significantly affect breathing patterns. Patients may experience nasal congestion, difficulty breathing through one or both nostrils, and a sensation of blocked airflow. This can lead to sleep disturbances, reduced exercise tolerance, and a diminished overall quality of life. Chronic breathing problems can impact social interactions, work performance, and general well-being. Furthermore, the deviation can contribute to chronic sinusitis and other related respiratory conditions.
Severity Levels of Deviated Septum Conditions
| Severity Level | Description | Breathing Impact | Potential Complications |
|---|---|---|---|
| Mild | Minimal deviation, slight nasal obstruction. | Minor breathing difficulty, primarily noticeable during exertion. | Potential for chronic rhinitis or occasional nosebleeds. |
| Moderate | Significant deviation, noticeable nasal obstruction. | Significant breathing difficulty, especially during rest or sleep. | Increased risk of sinusitis, sleep apnea, and other respiratory issues. |
| Severe | Extreme deviation, severe nasal obstruction. | Severe breathing difficulty, impacting daily activities. | High risk of chronic sinusitis, sleep apnea, and significant quality of life impairment. |
Procedures for Correcting a Deviated Septum
Several procedures are available to correct a deviated septum, each with varying levels of invasiveness and potential benefits. Surgical intervention, such as septoplasty, is often considered medically necessary when non-surgical methods prove insufficient. The choice of procedure depends on the severity of the deviation, the patient’s symptoms, and their overall health.
Insurance coverage for rhinoplasty, particularly when a deviated septum is present, is often dependent on the specific policy and the surgeon’s justification for the procedure. While a comprehensive understanding of the intricacies of insurance reimbursements can be challenging, exploring resources like a ball jelly maker recipe book ball jelly maker recipe book might reveal unexpected parallels in the meticulous preparation and precise execution required for both culinary and surgical endeavors.
Ultimately, consultation with a qualified insurance provider and plastic surgeon is crucial to determine eligibility for coverage.
Coverage for Deviated Septum Correction
Insurance coverage for a deviated septum repair can vary significantly, influenced by factors like the specific policy, the extent of the deviation, and the patient’s overall health. While some policies may fully cover the procedure, others may only partially cover it or exclude it entirely. Understanding the nuances of coverage is crucial for patients seeking this procedure.
Examples of Insurance Coverage
Insurance policies often consider the deviated septum correction as a medically necessary procedure when it significantly impacts breathing or causes related complications. Examples of coverage can range from full coverage for the surgery, including surgeon fees, anesthesia, and hospital charges, to partial coverage for certain components of the procedure. Some policies may require pre-authorization or prior approval from the insurer before the procedure can be performed.
It is essential to review the policy details to understand the specifics of the coverage.
Insurance coverage for rhinoplasty, particularly when a deviated septum is present, varies significantly depending on the specific policy and the extent of the needed procedure. Factors such as pre-existing conditions and the necessity of the procedure for medical reasons play a crucial role in determining coverage. To find suitable accommodations for a new living situation, exploring options for one bedroom apartments in Bowling Green, Ohio one bedroom apartments in bowling green ohio might be beneficial.
Ultimately, consulting with an insurance provider and a qualified medical professional is essential for obtaining accurate information regarding coverage for such procedures.
Case Studies of Successful Claims
Numerous successful claims have been made for deviated septum procedures. A common example involves a patient with chronic nasal congestion and headaches. After a thorough evaluation by an ENT specialist, a deviated septum repair was deemed medically necessary to alleviate the symptoms. The insurance company, upon review of the medical documentation and the specialist’s justification, approved the claim, resulting in full or partial coverage.
Another successful claim involved a patient experiencing recurrent sinusitis, which was directly linked to a deviated septum. The insurance company, recognizing the connection between the deviated septum and the recurring sinus infections, approved the claim for the surgical correction.
Documentation Requirements
Thorough documentation is crucial for a successful insurance claim. This includes detailed medical records outlining the patient’s symptoms, the diagnosis of a deviated septum, the justification for surgical intervention, and the surgeon’s recommendation for the procedure. Medical imaging, such as X-rays or CT scans, showing the extent of the deviation and its impact on nasal airflow, is typically required.
The surgeon’s detailed report outlining the procedure and its necessity is essential evidence. The insurer’s specific documentation requirements should be reviewed before initiating the claim process.
Reasons for Claim Denials
Insurance claims for deviated septum corrections can be denied for several reasons. Lack of proper documentation, including insufficient medical records, missing imaging reports, or unclear justification for the procedure, are common causes. The surgeon’s report not adequately demonstrating the medical necessity of the procedure, or if the deviation is deemed not severe enough to warrant surgery, can also lead to denial.
Finally, the procedure might be deemed cosmetic rather than medically necessary.
Table of Common Insurance Denials and Appeals Strategies
| Reason for Denial | Description | Possible Appeal Strategies |
|---|---|---|
| Insufficient Documentation | Missing or incomplete medical records, imaging reports, or surgeon’s notes. | Provide missing documentation, clarify any inconsistencies, or request a supplementary report from the healthcare provider. |
| Lack of Medical Necessity | The insurance company believes the procedure is not medically necessary to address the patient’s condition. | Highlight the impact of the deviated septum on the patient’s breathing, sinus health, or other related symptoms. Provide detailed evidence demonstrating the necessity of the procedure. |
| Cosmetic Procedure | The insurance company considers the procedure primarily cosmetic and not medically necessary. | Present clear evidence that the procedure is necessary to alleviate breathing problems or related symptoms, emphasizing its impact on the patient’s overall health. Include detailed reports from the surgeon and other specialists. |
| Pre-authorization Issues | The procedure was not pre-authorized before surgery. | Attempt to demonstrate why pre-authorization was not possible. If there were extenuating circumstances, explain those and provide any supporting documentation. |
Coverage Differences by Geographic Location
Coverage for deviated septum repair can vary significantly across different geographic locations. In some regions, insurance companies are more likely to approve claims for procedures deemed medically necessary. This can be influenced by regional healthcare standards, physician guidelines, and the prevalence of certain conditions. Policy differences between insurance providers within a region can also impact the outcome of claims.
Comparison of insurance policies and practices within a specific geographic area is recommended to understand the potential differences.
Cosmetic vs. Medical Rhinoplasty
Understanding the distinction between cosmetic and medical rhinoplasty is crucial for accurately assessing insurance coverage. While both procedures involve reshaping the nose, their motivations, goals, and medical justifications differ significantly. This understanding helps determine if a procedure falls under medical necessity or cosmetic enhancement.
Distinction Between Cosmetic and Medical Rhinoplasty
Cosmetic rhinoplasty, often referred to as a “nose job,” primarily aims to improve the aesthetic appearance of the nose. Patients seeking this procedure typically have concerns about the shape, size, or proportions of their nose, regardless of any functional impairment. Conversely, medical rhinoplasty addresses functional problems stemming from nasal deformities. These problems can include breathing difficulties, such as those caused by a deviated septum, or structural issues impacting airflow.
Overlap of Cosmetic and Medical Reasons
Sometimes, a nose job can address both cosmetic and medical concerns. A deviated septum, for instance, might not only cause breathing problems but also contribute to an aesthetically unappealing nasal profile. In such cases, the surgical correction often tackles both the functional and aesthetic aspects simultaneously.
Medical Criteria Differentiating the Procedures
Medical necessity for rhinoplasty hinges on demonstrable functional impairment. Documentation from a physician is paramount in justifying the procedure. Specific medical criteria typically include:
- Evidence of significant breathing difficulties, such as nasal congestion, snoring, or sleep apnea, directly attributable to a deviated septum or other nasal structural abnormalities.
- Documented impact on daily activities due to impaired nasal breathing, such as difficulty exercising or concentrating.
- Diagnosis and detailed description of the nasal deformity, specifying its impact on the patient’s respiratory system.
- Medical records showing that conservative treatments, like nasal sprays or other non-surgical interventions, have proven ineffective in alleviating the breathing issues.
Contrasting Cosmetic and Medical Rhinoplasty
| Characteristic | Cosmetic Rhinoplasty | Medical Rhinoplasty |
|---|---|---|
| Motivation | Aesthetic improvement; desire for a more pleasing nose shape | Correction of functional nasal problems; improvement of breathing |
| Goals | Enhancement of appearance; achieving a desired aesthetic result | Restoration of normal nasal function; improvement of breathing patterns |
| Typical Outcomes | Improved facial symmetry; enhanced nose shape | Improved breathing; reduced nasal congestion; relief from respiratory symptoms |
Importance of Physician Documentation
The physician’s documentation plays a critical role in distinguishing between cosmetic and medical rhinoplasty. Thorough medical records, including detailed patient history, physical examinations, diagnostic tests (if applicable), and treatment plans, are essential. The documentation should clearly establish the medical necessity for the procedure and the extent of the functional impairment. The documentation should also highlight the limitations of non-surgical interventions and the rationale for surgical intervention.
Justifying a Nose Job with Cosmetic Aspects
When a deviated septum correction is medically necessary but also has cosmetic aspects, the justification to insurance hinges on meticulous documentation. The physician must clearly delineate the medical necessity, emphasizing the impact of the deformity on the patient’s breathing and daily life. The cosmetic benefits should be secondary to the medical justification, clearly outlining how the procedure will simultaneously address both functional and aesthetic concerns.
Examples include cases where the nasal deformity directly affects the aesthetic profile, significantly impacting the patient’s self-esteem and social interactions. A detailed explanation of how the procedure directly alleviates breathing difficulties while simultaneously improving the patient’s appearance is critical.
Insurance Claim Process for Deviated Septum Repair

Navigating the insurance claim process for a deviated septum repair can be complex. Understanding the steps involved, required documentation, and potential appeals process is crucial for a smooth and successful outcome. This section details the typical procedure, ensuring you’re prepared for the administrative tasks.
Typical Claim Submission Steps
The process for submitting an insurance claim for a deviated septum repair generally involves these steps:
1. Pre-authorization
Contact your insurance provider to determine coverage and obtain pre-authorization. This step verifies that the procedure is covered and whether any specific pre-authorization forms or requirements are necessary. Pre-authorization often requires detailed medical information, including the diagnosis, proposed treatment, and expected costs.
2. Gathering Documentation
Compile all necessary documents, including medical records, physician’s orders, and pre-authorization forms. This includes your insurance card, policy information, and any relevant imaging results (X-rays, CT scans). Ensure all documents are properly completed and signed.
3. Scheduling the Procedure
Schedule the surgery after receiving pre-authorization. Confirm the details with the surgeon and insurance company to avoid any delays or complications.
4. Submitting the Claim
After the surgery, obtain the necessary paperwork and receipts from the medical facility. This might include a detailed surgical report, billing statements, and itemized charges. Submit these documents, along with the pre-authorization form, to your insurance company through the designated channels (often online portals or mail).
5. Receiving the Payment
Once the insurance company processes the claim, you’ll receive payment directly or have your account credited. This process can take several weeks or months, depending on the insurance provider’s processing time. Follow up with the insurance company if you don’t receive payment within the estimated timeframe.
Required Forms and Documentation
A claim for deviated septum repair typically necessitates the following:
- Pre-authorization form: This form requests the insurance company’s approval for the procedure. It usually includes details about the medical necessity of the surgery, the proposed treatment plan, and any required tests.
- Surgical report: A detailed account of the procedure performed by the surgeon. This report documents the diagnosis, treatment methods, and post-operative instructions.
- Billing statements and receipts: These documents provide a record of the charges incurred for the procedure, including pre-operative tests, the surgical procedure itself, and post-operative care.
- Medical records: Complete records of your medical history, including previous diagnoses, treatments, and any relevant imaging results.
- Insurance card and policy information: These documents are crucial for identifying the policyholder and verifying coverage details.
Handling a Denied Claim
If your claim is denied, it’s crucial to understand why. Review the denial letter carefully and take the following steps:
1. Understanding the Denial
Carefully examine the denial letter to understand the specific reason for rejection. Common reasons include lack of medical necessity, exceeding the benefit limit, or insufficient documentation.
2. Contacting the Insurance Company
Contact the insurance company to discuss the denial and obtain clarification. Explain the medical necessity of the surgery and any relevant information that might have been missed.
3. Appealing the Decision
If the initial denial is not satisfactory, initiate the formal appeal process. This typically involves submitting supporting documentation, such as additional medical records or statements from medical specialists, explaining the medical necessity of the surgery and why it was not properly assessed in the first denial.
Example Appeal Letter
[This section should include a sample letter to the insurance company requesting an appeal of a denied claim. The letter should be structured to address the specific reason for the denial, present supporting evidence, and request a reconsideration of the decision.]
Claim Process Flowchart
[This section should include a flowchart illustrating the claim process, including potential denials and appeals. The flowchart should visually represent the different steps, decisions, and possible outcomes. For example, it should show the path for a successful claim, the steps involved in appealing a denial, and the outcomes of different appeals. A well-designed flowchart will include clear labels for each step and decision point.]
Factors Influencing Insurance Decisions
Insurance coverage for a nose job related to a deviated septum is not always guaranteed. Several factors play a crucial role in determining whether the procedure will be covered. Understanding these factors empowers patients to proactively navigate the insurance process and increase the likelihood of approval. A thorough understanding of these factors is vital for successful claims.
Pre-Authorization’s Importance
Pre-authorization is a crucial step in the insurance process. Insurance companies require pre-authorization to ensure the procedure is medically necessary and aligns with their coverage guidelines. Failure to obtain pre-authorization may result in denial of the claim. This process involves submitting documentation to the insurance provider, including medical records, physician recommendations, and the proposed procedure details. The insurance company will review this information to assess the necessity and appropriateness of the procedure, often requiring specific criteria to be met.
This proactive approach ensures that the procedure is justified and compliant with the insurance policy.
Impact of Pre-Existing Conditions
Pre-existing conditions can significantly impact insurance coverage decisions. If a deviated septum is considered a pre-existing condition, the insurance company may apply different coverage criteria. The specifics of coverage vary greatly between insurance policies. A pre-existing condition may lead to a higher deductible, a reduced coverage amount, or even complete exclusion from coverage. It is essential for patients to disclose any pre-existing conditions during the initial consultation with their physician and the insurance company.
Patient’s Medical History and Physician’s Recommendation
The patient’s medical history and the physician’s recommendation play pivotal roles in the insurance decision-making process. A comprehensive medical history provides a detailed overview of the patient’s health status, including any previous surgeries, illnesses, or injuries. The physician’s recommendation, supported by detailed documentation of the patient’s need for the procedure, is a strong indicator of the procedure’s necessity.
The physician’s rationale and justification for the rhinoplasty, emphasizing the link between the deviated septum and the functional or aesthetic improvement, strongly influence the insurance company’s decision. The physician’s detailed report must clearly Artikel the medical necessity of the procedure and how it addresses the deviated septum and any associated complications.
Addressing Potential Concerns
Insurance companies may raise concerns about the necessity of the procedure. To address these concerns, it is essential to present compelling evidence. This includes detailed medical records, physician statements, and diagnostic tests. The physician’s statement must clearly articulate the relationship between the deviated septum and the patient’s symptoms, highlighting the functional impairment and the anticipated benefits of the procedure.
Thorough documentation, including detailed reports from the physician, diagnostic tests results, and X-rays, is crucial in justifying the procedure.
| Factor | Description |
|---|---|
| Pre-authorization | Essential step for insurance approval; ensures medical necessity. |
| Pre-existing Conditions | May affect coverage; detailed disclosure is critical. |
| Patient’s Medical History | Provides context for the procedure’s necessity. |
| Physician’s Recommendation | Crucial for demonstrating medical necessity. |
| Documentation | Thorough records and reports support the claim. |
Final Conclusion
In conclusion, securing insurance coverage for a nose job related to a deviated septum requires careful consideration of medical necessity and a thorough understanding of the insurance claim process. Documentation from your physician is critical. While outcomes can vary, being proactive and informed significantly increases the likelihood of a successful claim. Remember, individual circumstances and insurance policies can differ, so consulting with both your physician and insurance provider is essential.
Question & Answer Hub: Does Insurance Cover Nose Job With Deviated Septum
Does insurance cover all types of nose jobs?
No, insurance coverage varies widely. A nose job related to a medically necessary deviated septum has a higher chance of being covered than a purely cosmetic procedure.
What are common reasons for insurance claim denials?
Claims can be denied if the procedure isn’t deemed medically necessary, if pre-authorization isn’t obtained, or if documentation doesn’t adequately support the medical necessity.
How long does the insurance claim process typically take?
The timeframe varies greatly depending on the insurance company and the complexity of the claim. Expect to allow several weeks, potentially months, for the process.
What if my insurance claim is denied?
You have the option to appeal the decision. Thoroughly review the denial letter, gather additional supporting documentation, and craft a compelling appeal letter to the insurance company.
